Maintaining a Healthy Heartbeat
- Category: Heart & Vascular, Patient Stories
- Posted On:
Electrical impulses control the pace and rhythm of your heart around the clock, every day of your life. But like faulty electrical wiring in your home or car, problems with your heart’s natural electrical system can cause trouble. Heartbeats may speed up, slow down or become wildly irregular. These disturbances, or arrhythmias, can cause fatigue or fainting, boost risk for a stroke, or even be fatal.
One in 18 Americans has a heart arrhythmia. Some are brief and harmless; others are more serious. If you have one, you may feel nothing at all—or notice symptoms such as palpitations, lightheadedness, fatigue, chest pain, or shortness of breath.
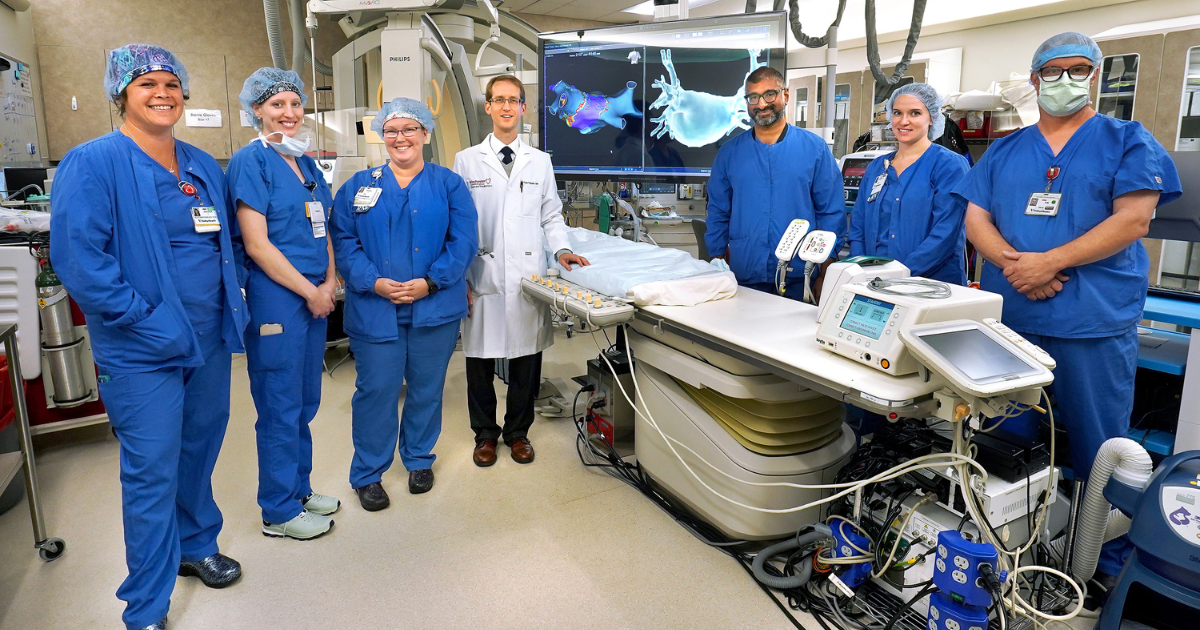
The Cardiac Electrophysiology Lab in Valley Health’s Heart & Vascular Center at Winchester Medical Center specializes in diagnosing and treating heart problems caused by arrhythmias. “Heart disease and high blood pressure are the leading causes of heart arrhythmias in the United States, but other disorders and genetics can also be responsible,” says cardiac electrophysiologist Daniel V. Alexander, DO, FHRS, FACC, medical director of the Winchester Medical Center Electrophysiology Clinical Council.
The lab, the first in the region when it opened in 2009, was the first in the state to be accredited by the Intersocietal Accreditation Commission (IAC) in cardiac electrophysiology—demonstrating Valley Health’s commitment to the highest-quality patient care for arrhythmias.
What happens there? “We follow and monitor patients and, when needed, treat arrhythmias with medications and with procedures such as ablation and the implantation of pacemakers, defibrillators and other devices,” says cardiac electrophysiologist Todd Teigeler, MD. The team also has a comprehensive device clinic that provides maintenance and monitoring of implantable cardiac devices and monitors. The clinic receives reports from a patient’s device via Bluetooth and provides remote analysis and detection of possible future complications. “It’s all to bring the heart back into a healthier rhythm and control risks so people can lead their lives with peace of mind.”
Here’s what to know about the most common types of arrhythmias:
Atrial Fibrillation: Controlling Offbeat Rhythms
Six years ago, Kip Walton discovered he had atrial fibrillation during a routine physical with his primary care doctor. “I was very heavy and out of shape, so I thought that was why I sometimes felt so tired and out of breath just carrying the vacuum cleaner up the steps or doing yardwork,” says Walton, 56, of Front Royal, Virginia. “But it was AFib. My heart sometimes felt like it was wobbling or racing fast. The really dangerous thing is that with atrial fibrillation, blood can coagulate in your heart. Clots can form and get pushed to the brain, causing a stroke.”
Atrial fibrillation (AFib) is the most common heart rhythm disorder, affecting about 20 million to 25 million Americans. About 60 percent of the electrophysiology team’s patients have AFib. The condition boosts risk for a stroke fivefold, Dr. Alexander says, due to blood clots that can form in a small thumblike pocket near the top of the heart called the left atrial appendage (LAA). Normalizing heart rhythm and preventing clots from forming and leaving the heart are top priorities in treating AFib, he says.
Walton’s treatment included medications to control his erratic heart rhythms and his often-fast heart rate that climbed as high as 160 beats per minute (normal is 60 to 100). He took blood-thinning medications to prevent blood clots. At the same time, Walton made lifestyle changes that led to losing 80 pounds and adopted a regular walking routine. “I felt better,” he says, “but my heart didn’t really go back into a normal rhythm until I had cardioversion”—a procedure that uses a brief, low-energy electrical impulse to reset the heart rhythm.
Walton later had several rounds of cryoablation in the WMC Electrophysiology Lab using a cold-temperature probe to disable cells in his heart that were sending out abnormal electrical signals. “AFib runs in my family, and mine is chronic and persistent,” Walton says. “My case is very stubborn. Dr. Alexander kept working with me to get good results. I’ve been in a normal heart rhythm for a year now and feel great.”
AFib-Related Stroke: Devices to Lower Risk
For some people with AFib, clot-discouraging blood thinners have downsides. “The first-line treatment is usually medical therapy, but some people may not tolerate blood thinners,” Dr. Teigeler says. “The drugs may not be right for them due to a higher risk for bleeding because of frequent falls in older adults or having a high-risk job with the chance for injuries. In those cases, if their individual stroke risk score is high enough, we consider another management option: closing off the left atrial appendage with a device such as Watchman FLX or Amulet.”
Pattie Good, 81, a retired school bus driver and grandmother of seven from Gore, Virginia, had a Watchman device implanted in her heart’s LAA in a minimally invasive procedure in August 2021. She uses a walker to navigate around the home she shares with her husband, Bud, age 83, a retired American Red Cross vice president. Good has no trouble cooking meals, doing laundry, cleaning, and entertaining family, but the blood thinners caused bruising, she says, “with the smallest bump against anything.” That made Watchman FLX a good option for her, she explains.
Watchman FLX looks like a little parachute. It’s fitted over the LAA in a minimally invasive procedure in which a small incision is made in the femoral vein at the groin, and the device is carefully threaded up to the heart. Good spent one night in the hospital and came home feeling fine. Recovery involved taking it easy for a few days—no driving or lifting heavy items.
But she’s not the only family member who has the device. Bud was diagnosed recently with AFib and had Watchman FLX implanted in October 2022. “We’re probably the only couple married 61 years who both have it,” Good says. “I know the Watchman is in my heart to protect me, and now to protect Bud, too. That’s a good feeling.”
Ventricular Tachycardia: Calming Fast Heartbeats
A smaller but still significant number of patients are monitored and treated as needed for a heart rate problem called ventricular tachycardia, when the heart races due to abnormal electrical activity from the bottom chambers of the heart.
“About 10 percent of our practice is managing ventricular arrhythmias,” Dr. Alexander explains, which are arrhythmias caused by irregular electrical signals in the lower chambers of the heart that prevent it from effectively pumping blood to the rest of the body. “This may be due to damage from a heart attack or other causes.”
Ventricular tachycardia, diagnosed in about 90,000 Americans each year, may cause lightheadedness and fainting. But it’s also the cause of 300,000 sudden cardiac deaths annually. “It’s a dangerous heart rhythm,” Dr. Teigeler says. “Ideally, we can start treating it before it leads to an episode where someone passes out or needs CPR.” Advanced testing, he says, helps determine the optimal treatment for those at highest risk. Therapies include medications to control heart rate, implantable cardiac defibrillators that automatically restart the heart, and ablation techniques to normalize heart rhythm by disabling heart cells sending out rogue electrical signals.
“Ablation for ventricular tachycardia is a very important component of what we do,” Dr. Alexander says. “These are some of our sickest patients. It used to be there wasn’t much we could do beyond medications and defibrillators. Now we have this important and effective option for management that makes a big difference.”
Bradycardia: Bringing Slow Beats Back to Normal
It’s unknown how many Americans have bradycardia—a heartbeat of 50 to 60 beats per minute or lower—but about 1 in 600 older adults, age 65-plus, have this slow heartbeat condition with symptoms such as shortness of breath, chest pain, fatigue, and lightheadedness. These are signs that your heart can’t pump enough blood and oxygen throughout the body. “Slow heart rates aren’t always a problem,” Dr. Teigeler says. Athletes, for example, may have a low resting heart rate. But when slow heart rates cause symptoms, they get in the way of everyday life.
“As you get older, your heart’s natural pacemaker in the sinoatrial node develops fibrosis—it’s like rust on the cables of your heart’s conduction system,” he explains. “If you’re 75 years old and your heart rate stays in the 40s when you’re active, instead of speeding up, you don’t feel good. Climbing stairs or keeping up with the grandchildren becomes a tough task.”
For people with a slow heartbeat that’s causing difficulties, implanted pacemakers that deliver an electrical current to your heart can bring the heart rate back to normal. Electrophysiologists on the Heart & Vascular team can also implant a newer type of leadless pacemaker in a minimally invasive procedure that sends the device through the leg vein to your heart. While traditional pacemakers are implanted in the chest and have electrical leads extending to the heart, leadless pacemakers are smaller and implanted directly in one of the ventricles of the heart. “This improves the symptoms and improves a person’s quality of life,” Dr. Teigeler says. “You can do what you love again.”
To learn more, visit valleyhealthlink.com/heart.


