Two Valley Health Hospitals Add Robotic Technology for Knee Replacement
- Category: Orthopedics
- Posted On:

Technology Offers Warren and Winchester Patients Personalized Precision Orthopedic Care
Valley Health orthopedic surgery teams at Warren Memorial Hospital (WMH) and Winchester Medical Center (WMC) have brought on two new surgical robots to help patients seeking relief from arthritic knee pain and immobility through total knee replacement.
Teams led by fellowship-trained orthopedic surgeons Mesfin Shibeshi, DO, at WMH and Max Lingamfelter, DO, at WMC, are using robotic technology to aid in same-day total knee reconstruction procedures at both facilities.
“The surgical robot is another enhancement to the comprehensive care our teams provide, from thorough pre-op patient education through surgery and post-op physical therapy, so our patients can get back to living life more fully, more comfortably, faster,” said Julie Miksit, BSN, MBA, Vice President, Operations and Service Lines at Valley Health.
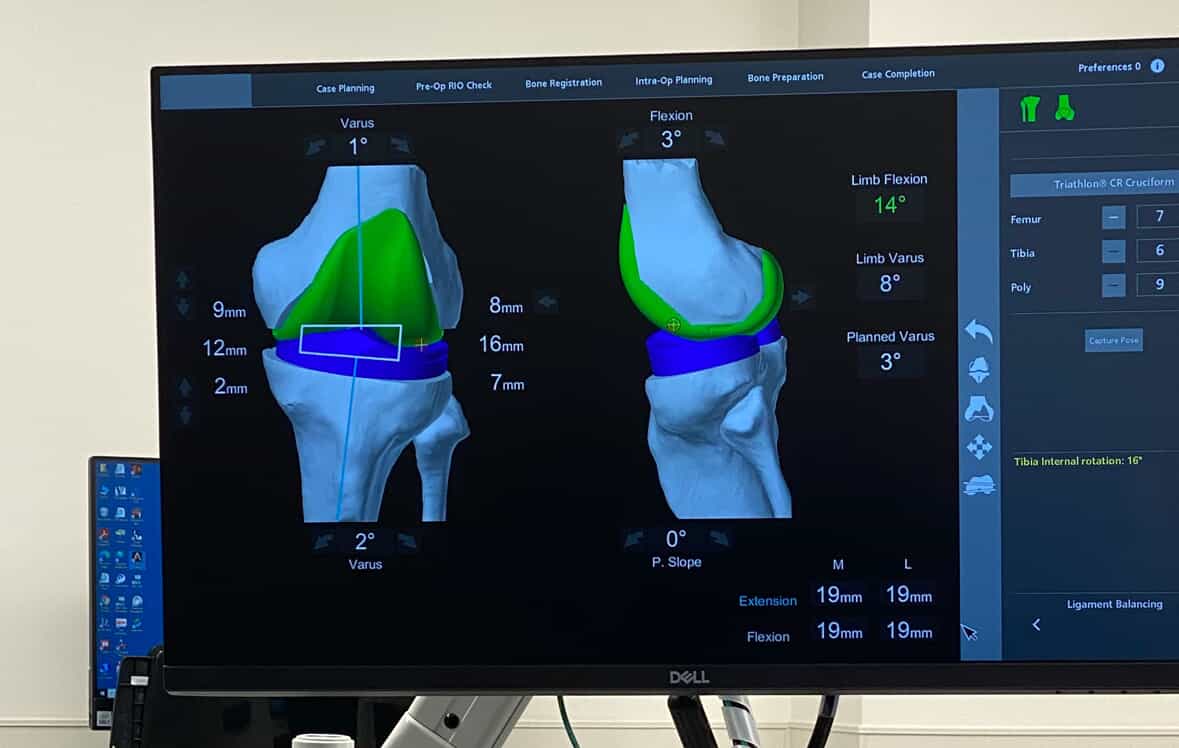
Robot-assisted surgery offers uncompromising steadiness and precision when performing total knee replacements. Paired with the robotic technology, an imaging and surgical planning interface provides a detailed 3D model of the patient’s unique anatomy, supporting more precise planning of incisions and implant placement before surgery. During the procedure, the surgeon can guide the robotic arm to achieve the predetermined surgical plan with a high level of accuracy, while also having the freedom to make intraoperative adjustments, if needed. This level of surgical personalization and precision can limit soft tissue damage, preserve bone, and reduce post-surgical pain for some patients.
About 25% of American adults have arthritis. It is a leading cause of work disability, with annual costs for medical care and lost earnings of $303.5 billion. Replacing a knee or hip joint damaged by osteoarthritis with a prosthesis is one of the most common orthopedic procedures. According to the American Academy of Orthopedic Surgeons (AAOS), 90% of people who have a knee replacement experience a significant reduction in pain.
The Valley Health orthopedics team completes more than 1,000 total joint replacement procedures each year, offering relief for those with joints damaged by degenerative arthritis, injury or wear and tear. Refinements in surgery, pain management and rehabilitation have continued to improve the overall experience. For many, joint replacement is now an outpatient surgery and patients go home the same day.
“The robot was an important addition to our orthopedic surgery program at Warren Memorial,” said Dr. Shibeshi. “The individualized 3D pre-planning is exceptional, and the robotic arm is a very stable, precision extension of the surgeon’s hands. We are excited to offer patients this advancement for the long-term relief of knee pain and immobility.” WMH was the first Valley Health hospital to earn the Gold Seal of Approval® for Total Knee Replacement and Total Hip Replacement Certification from The Joint Commission, recognizing its compliance with rigorous performance standards for safe, high quality joint replacement care. This certification attests to the quality of the hospital’s total joint program, from pre-surgical consultation and patient education, to surgery, pain management, rehabilitation and follow-up.
One of the first patients to benefit from the new robotic equipment at WMH was Front Royal resident Marie McDaniel, age 75, an avid walker despite severe arthritis and bone spurs. She has been very pleased with the personal care she has received from the whole team, before, during and after her mid-March outpatient surgery. “They’re the best of the best,” McDaniel said of the WMH team. “They still have small town caring and compassion, and give great medical, but also personal and psychological, care.” She began physical therapy at Valley Health’s Riverton Commons location with realistic expectations. “I’m not a patient person, but I have a wonderful physical therapist I absolutely adore,” she said.
Dr. Lingamfelter, as well as Dr. Shibeshi, is fellowship-trained and experienced in all levels of orthopedic surgery complexity. “Robotic-assisted surgery is the next evolution in total joint replacement and delivers a level of accuracy which is beyond the human eye,” said Dr. Lingamfelter. “Using this technology, we are able to plan and create a 3-dimensional model of the knee before the bone is cut, which allows us to predict how the knee will respond to these implants. This delivers a more consistent and reproducible feel to every knee and allows us to achieve this goal using the most conservative bony cuts.”
One of Dr. Lingamfelter’s patients, Trista Runion, 47, of Martinsburg, WV, had sustained multiple gymnastics injuries and previously struggled to hike and climb stadium steps at sporting events. “My knees are so bad I can’t do a lot of things. It’s especially hard to address being overweight when exercise is so painful,” she said. “Dr. Lingamfelter was very compassionate; he didn’t judge, he just wanted to help.” Runion has had very little surgical pain since her robotic procedure in March and has made tremendous functional gains throughout her postoperative recovery. “I’ve never felt this stable,” she said, adding that Dr. Lingamfelter’s robot-assisted team will replace her other knee in mid-May.
- For more information about orthopedic services at Valley Health, visit valleyhealthlink.com/ortho.
- To learn more about Dr. Lingamfelter, click here.
- To learn more about Dr. Shibeshi, click here.


